by Francesco M. Egro, MBChB, MSc, MRCS (@FrancescoEgro)
The July edition of the #PRSJournalClub offered an exciting discussion of a great PRS Journal article entitled “Multisite Lymphaticovenular Bypass Using Supermicrosurgery Technique for Lymphedema Management in Lower Lymhedema Cases” by Makoto Mihara, MD (@mihara_hara_lym), Hisako Hara, MD (@hara_lymph), Shuichi Tange, MS, Han Peng Zhou, MS, Mari Kawahara, MD, Yohei Shimizu, MD, and Noriyuki Murai, MD.
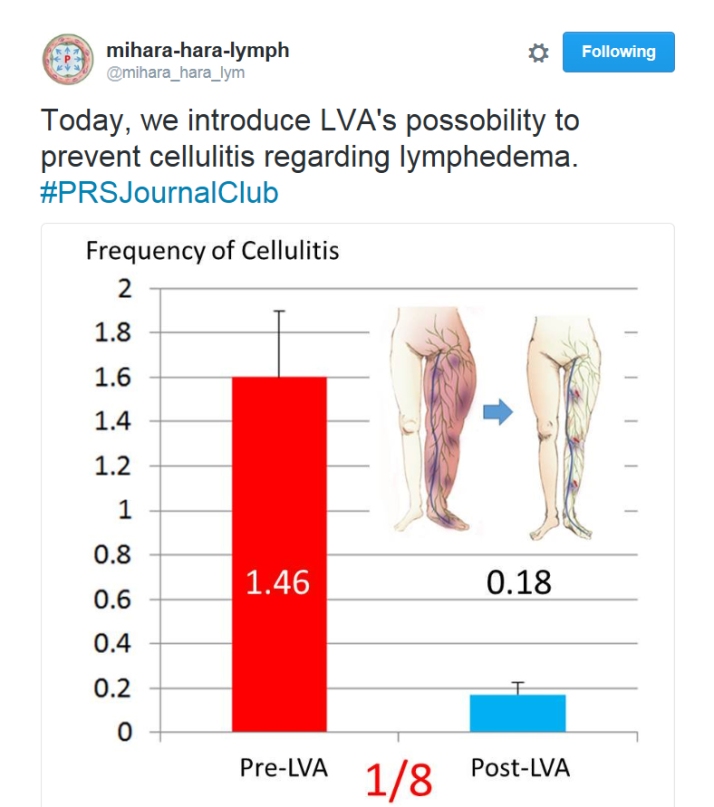
In the article, Mihara et al. reviewed retrospectively the outcomes of 84 patients (162 limbs; 73 female and 11 male patients) with lower limb lymphedema who underwent multisite lymphaticovenous bypass between August of 2010 and May of 2014. Postoperative examination showed that 67 limbs (47.7%) were classified as improved, 35 (27.3%) were classified as stable, and 32 (25%) were classified as worse. Postoperative interview revealed subjective improvement in 67 limbs (61.5%), no change in 38 (34.9%), and exacerbation in 4 (3.7%). The postoperative cellulitis rate was decreased to 0.13 times per year (p = 0.00084). Thus, the authors concluded that lymphaticovenous anastomosis is beneficial for lower limb lymphedema by improving limb circumference, subjective symptoms, and the frequency of cellulitis.
The article was first discussed in the PRS Journal Club podcast by the current Resident Ambassadors to the PRS Editorial Board Amanda Silva, MD (@AmandaKSilvaMD), Sammy Sinno, MD (@sammysinnoMD) and Raj Sawh-Martinez, MD (@docrfsm) with special guest moderator Babak Mehrara, MD. Listen to the discussion:
A vivid online discussion took place on twitter over a two-day period (July 17-18), where established plastic surgeons and residents were able to ask questions, and get answers from the authors of the article themselves! Don’t worry if you missed it! A summary of the exciting discussion is provided below divided into three sections for your convenience: 1. Top Q&A, 2. Pearls and articles shared by the authors, and 3. Beautiful dissection photographs shared by the authors.
Enjoy it and see you all at the next PRS Journal Club!
1. Top Q&A
@JordanFreyMD Jul 17: When do you prefer to perform lymph node transfer over LV bypass?
@hara_lymph Jul 17: We prefer LVA when we can find functional lymphatic vessels in lymphoscintigraphy or ICG lymphography, and lymph node trasfer would be better if we can’t find them
@shujashafqatmd Jul 17: so you prefer LVA or VLNT?@hara_lymph Jul 17: LVA can be performed under local anesthesia, and has no risk of donor site lymphedema. It msy be less invasive than LNT.
@AmandaKSilvaMD Jul 17: @shujashafqatmd believe what @hara_lymph means: if functional lymphatics remain try LVA, if scarred/non-functional do VLNT@AmandaKSilvaMD Jul 17: you think any other criteria for LVA vs. lymph node transfer?
@ChadPurnellMD Jul 17: how soon postoperatively can patients consider stopping compression garments?
@hara_lymph Jul 17: We usually recommend patients to try reduce elastic stocking about 6 mo after op. The effect of LVA appears gradually.@mihara_hara_lym Jul 17: We stop compression garment over 6 months after LVA, when our patients want stocking free. We need to check patients’ condition 6 months after stocking free. If the condition is worse, we start stocking again.
@ChadPurnellMD Jul 17: how do you predict Maegawa stage 5 #lymphedema patients who will still have ectasis vessels?
@mihara_hara_lym Jul 17: You know that Maegawa stage 5 cases are very difficult. And we check lmph vessels very carefully using ICG lymphography.
@AmandaKSilvaMD Jul 17: what about pts moving under local? Such a meticulous/fine surgery seems tough with moving target!
@mihara_hara_lym Jul 17: Our 1st option is LVA under local anaesthesia. 2nd option is other lymphatic surgery. Low invasiveness is very important.@hara_lymph Jul 17: Usually the patients’ moves count for nothing!
@shujashafqatmd Jul 17: Any oral anxiolytics/narcotics prior to the procedure?@hara_lymph Jul 17: No anxiolytics is needed. We rather want patients to stay awake to check the condition of their own lymphatic vessels!
@AmandaKSilvaMD Jul 17: any technical pearls for working with ICG?
@mihara_hara_lym Jul 17: Our patients want to watch monitor of LVA during operation. And they understand their conditions of lymphatic vessels. @hara_lymph Jul 17: We show pt the monitor of microscope during op, so patients can easily understand the importance of stay still during LVA!
@shujashafqatmd Jul 17: That must come from detailed pre operative discussions!
@mihara_hara_lym Jul 17: Before the operation, our patients know traditional information of lymphedema. After operation, they know newest one.
@shujashafqatmd Jul 17: why do you think you had better volume reduction in late stage (contrary to previous studies)?
@mihara_hara_lym Jul 17: Severe patients know their dysfunction of lymph vessels during LVA. Postoperatively, they contend with illness seriously.
@danielzliu Jul 17: Totally agree with you!
@danielzliu Jul 17: Have you had more success with finding suitable lymphatic for #LVA on medial leg vs lateral?
@mihara_hara_lym Jul 17: Lymphoscintigraphy and ICG lymphography are very important before LVA. Based on them, we decide LVA site.
@hara_lymph Jul 18: We can find good lymphatic vessels at both medial and lateral leg. Preop examination is very important.
@pallabc Jul 17: How many sutures to accomplish End to End anast? 03? 04? Do you need any anti coagulation for the procedure?
@hara_lymph Jul 17: We usually make 4-6 sutures for 0.5-1.0 vessels. No anticoagulant postop.
@pallabc Jul 17: How messy is the lymphatic fluid welling up in the wound during anastomosis?
@hara_lymph Jul 17: Sometimes lympahtic fluid springs up from lymphatic vessels and a bit messy, but it means the lymphatic function is good!
@pallabc Jul 17: Any lymphorrhoea later after closure of the wound?
@hara_lymph Jul 17: We sometimes experience lymphorrhea in cases for whom preoperative compression therapy failed. Usually it does not happen.
@AmandaKSilvaMD Jul 17: do you have a preference for end-to-side or end-to-end for LVA?
@hara_lymph Jul 17: We prefer end-to-end. It will prevent lymphatic flow into the injured lympahtic vessels, if E-to-E LVA is placed distally.
@pallabc Jul 17: How is it possible to confirm the patency of anastomosis on table? By color? Acland?
@hara_lymph Jul 17: Intraoperative patency can be seen in the movie below. Please see 4:50-5:10 of the movie.
@danielzliu Jul 17: Distal injection of isosulfan blue dye for lymphatic identification and patency test. ICG also works
@pallabc Jul 17: So is there some preparation to be done like some length of compression therapy pre op or the patient comes to table after ICG?
@mihara_hara_lym Jul 17: Before LVA, we perform ICG, Statvein and Ultrasonography for detecting suitable vessels. Now we can detect them.
@danielzliu Jul 17: What’s the largest size mismatch you have done for end-to-side #LVA?
@AmandaKSilvaMD Jul 17: @danielzliu about 1:3 or 4 I’ve never formally measured & can’t speak for much more vast experience my attending has
@docrfsm Jul 17: what is the advantage of change rate vs circumference to track changes in lymphedema?
@hara_lymph Jul 17: So we prefer change rate to simple circumference changes.@pallabc Jul 17: If the procedure so effective & easy in your hands, would you offer it upfront at the time of mastectomy/breast reconstruction. After all, it’s just some procedures added to the upper limb away from the main dissection with no disturbance. Prophylactic!
@DannyBalkin Jul 17: How does history of radiation therapy effect your preop planning & postop outcomes?
@mihara_hara_lym Jul 17: Radiation destroy lymphatic function and anatomy. Use lymphoscintigraphy and ICG preoperatively to detect good lymphatics!
@hara_lymph Jul 17: Lymphatic function in radiated area is destroyed, so we plan LVA at more distal areas. That is effective.
@sammysinnoMD Jul 18: do you wrap immediately postop?
@AmandaKSilvaMD Jul 18: we wrap postop LVA for a month to avoid shear w/ garment. @mihara_hara_lym @hara_lymph you?
@hara_lymph Jul 18: We formerly start elastic garment 2 wk postop. Now we start weak compression at POD1, usual compression garment at POD2.
@pallabc Jul 18: But you said earlier that you don’t anti coagulate. Any reason?
@hara_lymph Jul 18: There is a little evidence about thrombosis prevention by anticoaglant for both blood vessels and lympahtic vessels…
@pallabc Jul 18: How long do you think before LVA is considered mainstream? Or is it already?
@hara_lymph Jul 18: So far, evidence on LVA is insufficient. This is reason why LVA is not mainstream, though it is very low invasive method.
@hara_lymph Jul 18: Now we are establishing the evidence on LVA, and we believe it will be widespread over the world in several years.
@pallabc Jul 18: Isn’t it counter intuitive, compression over a delicate anastomosis? Your earlier protocol more logical.
@hara_lymph Jul 18: Postop garment is 10mmHg and lymphatic inner pressure is over 30mmHg. Thinking logically, it may be OK.
@drAAmaldonado Jul 18: ICG injection could be painful for patients.Do u use any dilution? THX for the great #PRSJournalClub
@hara_lymph Jul 18: We usually inject small amount of xylocaine subcutaneously before injecting ICG. Pain can be reduced.
@sammysinnoMD Jul 18: ever a problem with patients moving during procedures under local?
@shujashafqatmd Jul 18: is there a protocol for choosing who gets isolated vs combined therapy and which therapies?
@hara_lymph Jul 18: We perform LVA for 1st option, because it is low invesive. If there is no functional Lympahtic vessel, LNT.
2. Pearls and articles shared by the authors
@FrancescoEgro Jul 17: Are you working with Prof. Campisi too?
@mihara_hara_lym Jul 17: We visited Campisi’s hospital 3 y ago. Campisi’s procedure and our procedure are different. Now, we try to blend them !!
@AmandaKSilvaMD Jul 17: what did you adopt from Campisi’s methods?
3. Beautiful dissection photographs shared by the authors